
16 . 04 . 2020
Polycystic Ovary Syndrome - What is it? - Part I
This syndrome is the most common hormonal disorder of the reproductive system in women. It is estimated to affect about 5-10% of women of childbearing age. The pathophysiology of this syndrome is complicated and there are several contributing factors. In this article, we will explore the various mechanisms that can lead to the typical Polycystic Ovary Syndrome (PCOS) symptoms.
To start, the name assigned to this syndrome is probably not the most adequate, since it leads us to think that the problem lies in the polycystic morphology of the ovary, when the latter is just a consequence of hormonal imbalance. In fact, PCOS is characterized by a state of increased androgen (male sex hormones) production, which affects the menstrual cycle and triggers a cascade of other events. It is important to note, however, that under normal conditions, male hormones are also present in women and have important functions in mood, libido and bone health, among others.
What are the symptoms of PCOS?
The most common symptoms are:
- Irregular (oligomenorrhea) or absent periods (amenorrhea) – generally the cycles are longer than 35 days.
- Hirsutism – excessive hair growth in “unwanted” areas for women, such as the chin, upper lip area, abdomen and inner thighs.
- Acne – especially in adult years. In teenagers, acne is a common feature.
- Alopecia – thinning and hair loss.
- Infertility – due to the lack of ovulation.
- Excess weight – more common than in the rest of the population.

Fig. 1 – Acne and hirsutism are two of the symptoms of PCOS caused by androgen excess.
How can the diagnosis be made?
According to the criteria of the Society for the Excess of Androgens and PCOS (AE-PCOS), the patient must fulfill the following criteria :
- Hyperandrogenism (excess of male sex hormones) – clinical (hirsutism, acne and alopecia) or biochemical signs (increased testosterone levels).
- Ovarian dysfunction – Irregular or absent periods; or evidence of polycystic ovaries on ultrasound.
- Exclusion of other conditions that cause excess androgens – drugs (oral contraceptives, antipsychotics, etc.), virilizing tumors, hypothyroidism, and others.
In teenagers, the diagnosis is more difficult, because it is normal for menstrual cycles to be longer and irregular, the ovaries can have a polycystic aspect on ultrasound and acne is also a common phenomenon. In this age bracket, the diagnosis should rely more on serum androgen measurement.
What are ovarian cysts due to?
At the beginning of each menstrual cycle, the ovarian follicles begin to develop, stimulated by the pituitary hormone FSH. Under normal circumstances, one of these follicles will dominate, cause the others to regress, and ovulation ensues. On the other hand, when hormonal stimuli are not concerted, ovulation does not occur, and the ovaries may have a polycystic appearance due to the presence of many developing follicles.
The term polycystic is used when more than 25 follicles in the ovary are visualized. However, this appearance is not necessarily pathological and can occur in 25% of healthy women (at certain stages of the menstrual cycle).
We therefore conclude that, even though polycystic ovaries are an important clue, their presence is not mandatory for the diagnosis of PCOS to be made.
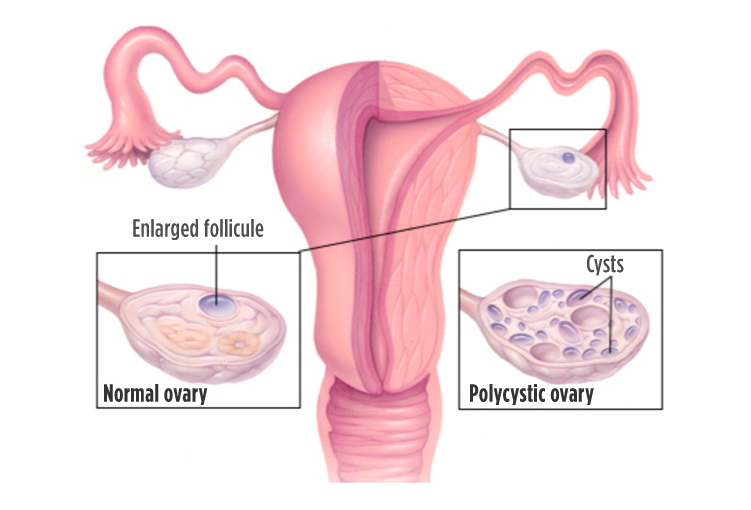 Fig. 2 – The typical polycystic morphology of PCOS is due to the presence of multiple developing follicles the ovary.
Fig. 2 – The typical polycystic morphology of PCOS is due to the presence of multiple developing follicles the ovary.
What causes PCOS?
This is the fundamental question, and the answer is not fully known. There seems to be a segment of the female population with a genetic predisposition for the overproduction of androgens. When external factors promote the expression of such genes (epigenetics), the problem will then manifest.
There are four main categories of triggering events that we will analyze separately:
- Insulin resistance
- Interruption of oral hormonal contraceptives
- Inflammation
- Excess adrenal androgen production
1. Insulin resistant PCOS
This is the most frequent cause of PCOS and occurs in about 70% of cases, being more common in women who are overweight (although this is not an essential condition). Insulin resistance is a complex condition, in which the body has difficulty using all the glucose in circulation, and so it increases insulin levels (hormone that promotes the entry of sugar into cells) to restore adequate concentrations.
Elevated insulin levels promote excess male sex hormones and ovarian dysfunction through the following mechanisms:
- increased ovarian production of androgens
- change of the secretion patterns of the pituitary hormone LH – this causes dysregulation of the menstrual cycles
- decreased synthesis of sex hormone-binding globulin (SHBG) by the liver – this protein binds to sex hormones (including testosterone). Only the free fraction (not bound to SHBG) of the sex hormones is active. Thus, by decreasing SHBG, the free (active) fraction of androgens increases.
Women with PCOS have a higher risk of developing Type 2 Diabetes Mellitus, which is also caused by insulin resistance.

Fig. 3 – Insulin resistance is more common in obese women, but it can also occur when the weight is normal.
2. Post contraceptive pill PCOS
Some women, after stopping the “pill”, don’t get their period back. In fact, hormonal contraceptives are effective because they suppress ovulation. After interrupting these medications, there may be a transient excess of male sex hormones, due to the following processes:
- oral contraceptives cause insulin resistance, which, as we saw above, interferes with ovulation and androgen production.
- most contraceptive pills have an intrinsic androgenic effect (varies depending on the progestin used). After the interruption, the body responds with an increase in the production of endogenous androgens.
To include a patient in this category of PCOS, she must have had normal menstrual cycles before starting the pill.
3. PCOS due to inflammation
In this group of women, the main stimulus for the production of male sex hormones stems from the chronic inflammatory load, which can sometimes be “silent”. The release of inflammatory cytokines such as interleukin 6 (IL-6) and tumor necrosis factor α (TNF-α) directly promotes the production of androgens in the ovaries.
The inflammation, and consequent oxidative stress, also contributes to insulin resistance, thus aggravating the situation.
This category of PCOS also includes problems arising from exposure to environmental toxins with an endocrine disruptor effect (external factors that “confuse” the hormonal system).
It is important to look for hidden sources of inflammation in these patients, such as: irritable bowel syndrome and intestinal dysbiosis, autoimmune diseases, chronic dental infections, etc.
4. Adrenal PCOS
This category covers about 10% of PCOS cases. So far we have been talking about testosterone which is the main androgen. However, there are other androgens in women, namely, 5-dihydrotestosterone (5-DHT), androstenedione and dehydroepiandrosterone (DHEA). DHEA is mostly produced in the adrenal glands. The sulfated form of this hormone (DHEA-S) is the marker generally used to quantify the production of adrenal androgens.
Most women with PCOS have elevation of all androgens. Nonetheless, in about 10% of cases, testosterone and androstenedione levels are normal, while DHEA-S (adrenal) levels are increased and are responsible for symptoms.
In these women, there seems to be an exaggerated response of the adrenal glands to pituitary stimulation with ACTH (messenger that acts on the adrenal glands, increasing their hormonal output) . Although the mechanism is not fully known, there is evidence that psychological stress influences the release of DHEA by the adrenal glands. Factors such as insulin resistance and inflammation are not directly involved in this process.
We learned about the symptoms, diagnostic criteria and main causes of PCOS. In the next article we will look at the therapeutic options available.
References:
- Goodman NF, Cobin RH, Futterweit W, Glueck JS, Legro RS, Carmina E. AMERICAN ASSOCIATION OF CLINICAL ENDOCRINOLOGISTS, AMERICAN COLLEGE OF ENDOCRINOLOGY, AND ANDROGEN EXCESS AND PCOS SOCIETY DISEASE STATE CLINICAL REVIEW: GUIDE TO THE BEST PRACTICES IN THE EVALUATION AND TREATMENT OF POLYCYSTIC OVARY SYNDROME – PART 1. Endocrine Practice. 2015;21(11):1291-1300.
- Goodman NF, Cobin RH, Futterweit W, Glueck JS, Legro RS, Carmina E. AMERICAN ASSOCIATION OF CLINICAL ENDOCRINOLOGISTS, AMERICAN COLLEGE OF ENDOCRINOLOGY, AND ANDROGEN EXCESS AND PCOS SOCIETY DISEASE STATE CLINICAL REVIEW: GUIDE TO THE BEST PRACTICES IN THE EVALUATION AND TREATMENT OF POLYCYSTIC OVARY SYNDROME – PART 2. Endocrine Practice. 2015;21(12):1415-1426.
- Goodarzi MO, Carmina E, Azziz R. DHEA, DHEAS and PCOS. Journal of Steroid Biochemistry & Molecular Biology. 2015;145:213-225.
- Briden, L. The Period Repair Manual 2nd Edition. CreateSpace Independent Publishing Platform, 2017.