30 . 08 . 2018
Lipoprotein (a) - An important cardiovascular risk marker
Despite significant advances in the diagnosis and therapy, cardiovascular disease in its various forms (coronary artery disease, stroke, peripheral artery disease) continues to be the leading cause of death in the industrialized world. Although some risk factors are non modifiable, like age and family history, there are several others to consider.
First of all, it’s important to clarify that, although it isn’t the only culprit in the pathogenesis of cardiovascular disease, cholesterol (more accurately the lipoproteins that carry it in the bloodstream) is an important risk factor. Lipid disorders can be broadly divided into 4 clinical categories:
- Elevated LDL (low-density lipoprotein)
- Low HDL (high-density lipoprotein)
- Elevated triglycerides
- Elevated lipoprotein (a)
Among these categories, Lp(a) has deserved less attention but the current information suggests its importance as an important independent risk factor for cardiovascular disease and calcific aortic valve sclerosis (pathology where calcium deposition on the aortic valve leaflets compromises blood flow).
What is lipoprotein (a)?
Lp(a) was identified in 1963 and it’s a type of lipoprotein in which a molecule of apoprotein(a) is bound to the apolipoprotein B100 (present in all LDL’s). Thus, it is similar to LDL but contains an additional molecule – apo(a) – that confers it a different structure and function. The molecular structure of Lp(a) is very similar to that of plasminogen, which is a fundamental protein for fibrinolysis (blood clot dissolution process). The apo(a) coding gene – LPA – is located in chromosome 6 and there are several known polymorphisms that genetically determine the concentration of Lp(a) in a given individual’s blood.
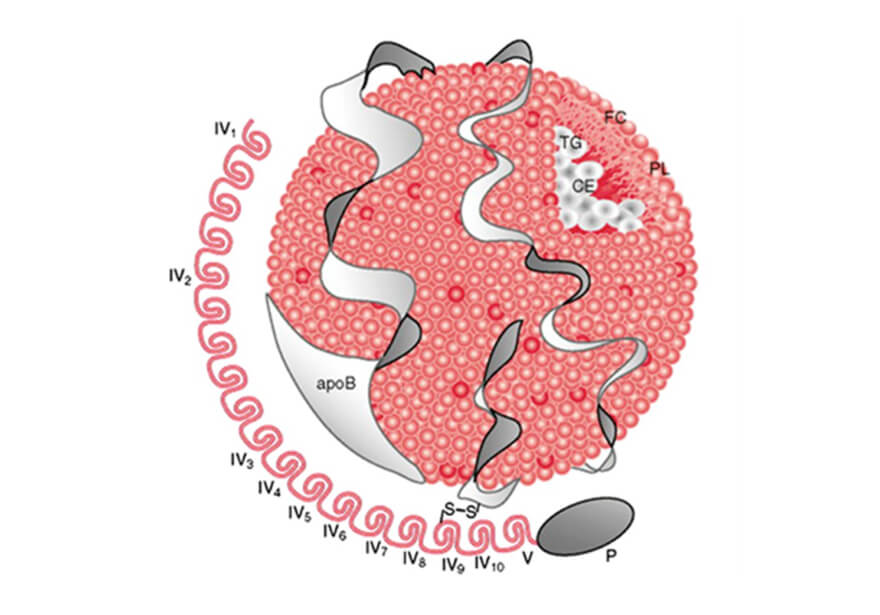
Fig. 1 – Structure of Lp(a) depicting the apo(a) linked to apoB100, the signature apolipoprotein associated with LDL particles.
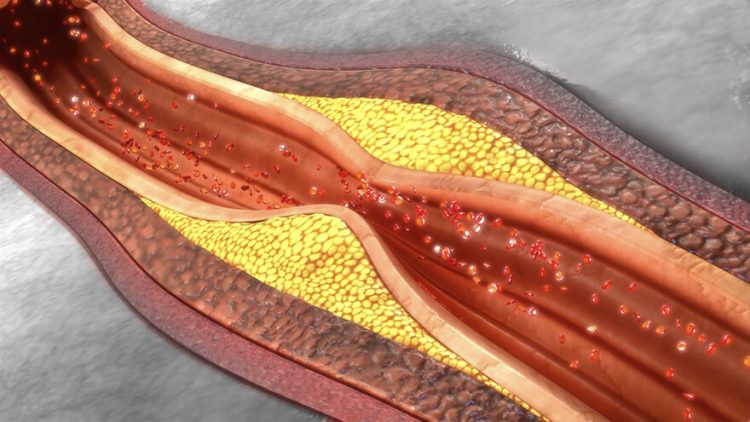
What is its role in atherosclerotic disease?
Aside from sharing the atherogenic risk of LDL’s, the additional apo(a) confers Lp(a) a larger pathogenic potential. The main properties that make Lp(a) more problematic are:
- Increased susceptibility to phospholipid oxidation, thereby increasing the inflammatory effect.
- Greater affinity for endothelial binding, contributing to its reactivity and dysfunction.
- Increased expression of adhesion molecules and inflammatory cytokines.
- Promotion of phagocytosis by macrophages, which leads to intracellular lipid accumulation and the formation of “foam cells”, key players in atherosclerosis.
- Inhibition of plasminogen activation, due to its structural similarity, interfering with the fibrinolytic system.
What is the normal range for blood levels of Lp(a)?
There is a significant variation amongst individuals for this specific marker. Plasma levels below 30 mg/dL (equivalent to 75 nmol/L if the particle number is measured instead of the concentration) are considered normal.
Studies show that one in five individuals has Lp(a) levels above 50 mg/dL (80th percentile), and one in four above 30 mg/dL (75th percentile).
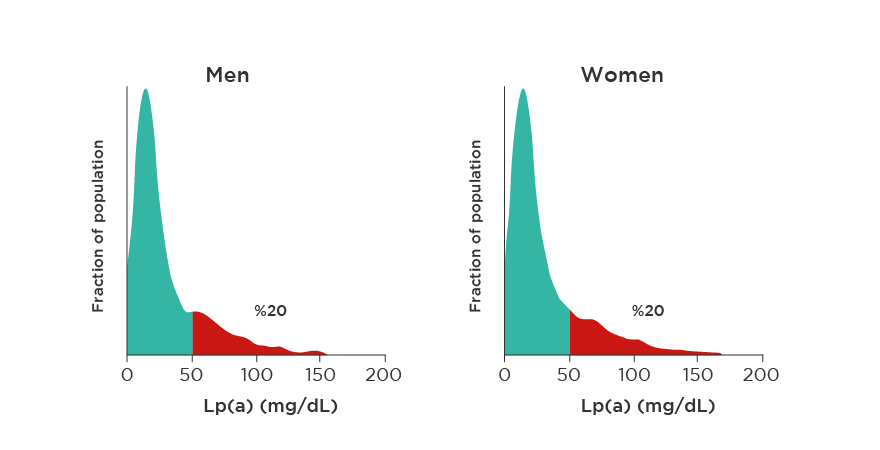
Fig. 2 – Distribution of Lp(a) levels in the caucasian population.
How does Lp(a) affect cardiovascular risk?
The medical literature confirms the association between Lp(a) levels and coronary artery disease, as well as calcific aortic valve stenosis. This is a continuous association, and independent of other risk factors.
The relative risk varies according to the different population studies. For instance, a prospective danish study found that individuals with plasma Lp(a) levels above 50 mg/L had a 2 to 3 – fold increase risk of acute myocardial infarction.
When LDL is also high, the risk increases significantly. However, recent studies in statin treated patients, showed that Lp(a) elevation contributes to increased cardiovascular risk, even if LDL is “at goal”.
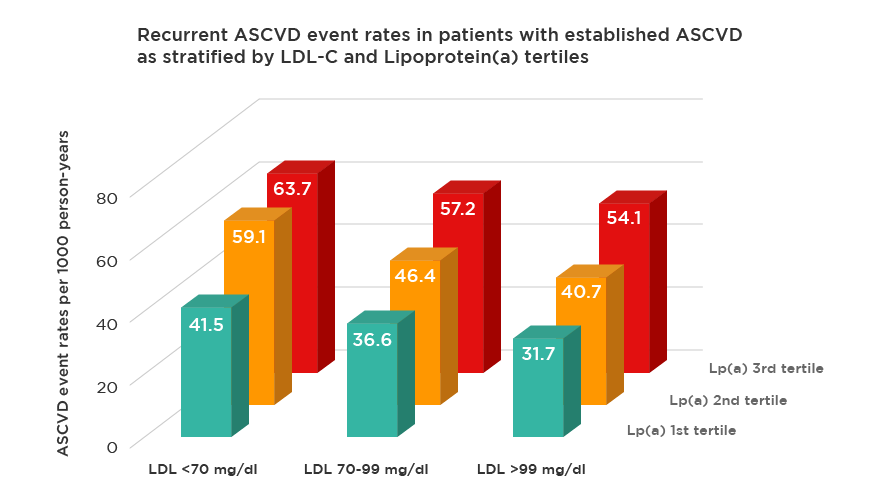
Fig. 3 – In patients with history of atherosclerotic cardiovascular disease on statins, despite being at target LDL-C levels, Lp(a) remain associated with increased risk.
Who should be tested?
The European Society of Cardiology recommends Lp(a) screening in individuals with high cardiovascular risk or a strong family history of premature atherosclerotic disease <55 years old for men and <65 years old for women), and in those with recurrent cardiovascular events despite lipid lowering therapy.
Nevertheless, being cardiovascular disease the leading cause of death, one can argue that everyone who is interested in knowing their risk and adjusting their lifestyle accordingly, should have their Lp(a) tested.
Lp(a) tends to be stable throughout an individual’s life span in the absence of specific therapeutic interventions (according to the literature, diet changes and/or statins do not influence Lp(a) levels). Therefore, a screening level below 30mg/dL excludes Lp(a) as an important risk factor for a given individual.
What to do when Lp(a) is elevated?
Even though there is an independent association between Lp(a) levels and cardiovascular disease, there aren’t clinical trials yet, showing that lowering Lp(a) leads to a reduction in cardiovascular events. This difficulty is inherent to the absence of good therapeutic options when it comes to lowering Lp(a) levels. The currently available drugs only provoke a modest Lp(a) reduction (20-30% maximum), specifically niacin and the PCSK9 inhibitors.
However, until a more effective Lp(a) lowering drug is developed, this information should be used to more accurately stratify people according to their cardiovascular risk, and aggressively control the remaining risk factors.
References:
Tsimikas S. A Test in Context: Lipoprotein(a): Diagnosis, Prognosis, Controversies, and Emerging Therapies. Journal of the American College of Cardiology (2017), 69:692-711
Ellis K., Watts G. Is Lipoprotein Ready for Prime-Time Use in the Clinic? Cardiology Clinics (2018), 36:287-298
Jacobson T. Lipoprotein(a), Cardiovascular Disease, and Contemporary Management. Mayo Clinic Procedures (2013), 88:1294-1311
Kamstrup PR., Benn M., Nordestgaard BG. Extreme lipoprotein(a) levels and risk of myocardial infarction in the general population: the Copenhagen City Heart Study. Circulation (2008), 117(2):176-84