16 . 09 . 2019
Fatty Liver - A Silent Epidemic
Non-alcoholic liver disease is an increasingly common entity and is expected to be the leading cause of liver transplantation in the near future.
The association between alcohol consumption and fat accumulation, under the form of triglycerides, in the liver is well established. However, this process is not exclusive to alcohol, and metabolic problems linked to insulin resistance can cause similar changes. When the patient has a fatty liver in the absence of alcohol consumption, the condition is referred to as “Non-Alcoholic Fatty Liver Disease” (NAFLD).
What is the prevalence of this disease?
At present, it is estimated that about 25% of the world’s population has NAFLD, which corresponds to an accumulation of at least 5% of the total liver mass in triglycerides. The prevalence is higher in patients with obesity (50%) and in those with type 2 diabetes mellitus (70%), which reflects the importance of insulin resistance in the development and progression of this condition.
What causes NAFLD?
The liver is the most important organ from the metabolic standpoint. One of its functions is to store energy in the form of glycogen and to produce triglycerides, which can be used as an energy source or reserve in other tissues. In the presence of a high-calorie diet, particularly rich in refined carbohydrates, a hyperinsulinemic state ensues and leads to excessive fat production in the liver. Fructose is a type of sugar present in fruit, but in higher proportions in refined sugar (about 50% of sugar is composed of fructose), and it is especially harmful to the metabolism. In parallel, if there is a deficiency of the nutrients involved in fat (triglycerides) export from the liver, in their specialized carriers – lipoproteins (VLDL) – the problem gets worse.
What is the clinical course of the disease?
NAFLD is often asymptomatic, which precludes an early diagnosis, most of the times. In its early stage, there is fat accumulation in the liver without inflammatory changes, and this is called simple steatosis. However, 20-30% of patients go on to develop inflammatory changes in the liver, with hepatocyte injury and fibrous tissue formation. This advanced stage of the disease is called non-alcoholic steatohepatitis (NASH), and 7-25% of these cases may progress to liver cirrhosis.
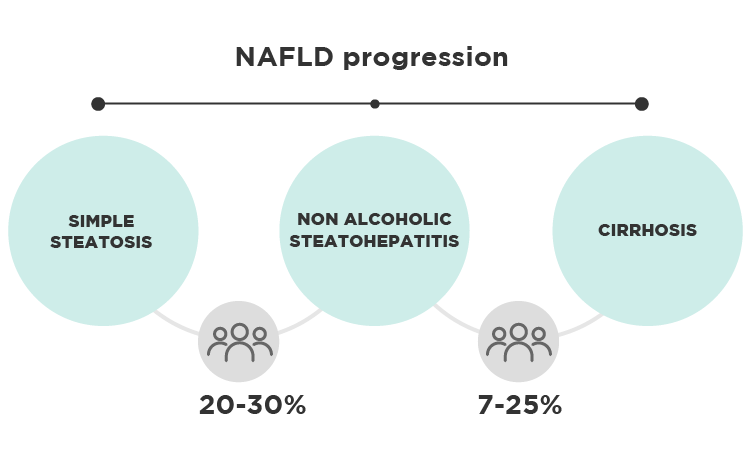
Figure 1 – Schematic representation of NAFLD progression

Figure 2 – Changes in the anatomical structure of the liver during the various stages of NAFLD.
How is NAFLD diagnosed?
In the steatosis phase, without inflammatory changes, the liver function tests (ALT, AST, GGT, etc.) are normal in 80% of the cases, which renders them unuseful for the diagnosis. Imaging studies are, therefore, essential in the diagnosis of NAFLD, and the options range from ultrasound to magnetic resonance imaging. Ultrasound is a more accessible exam and should be the initial choice. When there is steatohepatitis, liver function tests tend to be altered. However, a definitive diagnosis is made only by liver biopsy.
What is the treatment for this condition?
Being NAFLD a metabolic disorder, it is logical that the initial approach focuses on this area. When patients are overweight, which happens in the majority of cases, loss of, at least, 10% of body weight is recommended. A low-calorie diet high in protein and fiber and low in sugars and saturated fats is a good option in these cases. Some nutrients are particularly important, such as the following:
- Choline – one of the B-complex vitamins. It serves as the precursor for phosphatidylcholine, which is a phospholipid present in the lipoprotein membrane. Choline deficiency leads to insufficient production of lipoproteins in the liver, and consequent inability to export triglycerides from the liver. This nutrient is present in greater quantity in egg yolks and animal organs, particularly liver.
- Vitamin E – the main fat-soluble antioxidant in the body. The richest foods in vitamin E are nuts and seeds.
- Omega-3 polyunsaturated fatty acids (PUFA’s) – eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) have anti-inflammatory properties and promote insulin sensitivity. Their main source in the diet is fatty fish.
Physical activity is also crucial as it leads to an increase in lean mass and helps in reversing insulin resistance.

Fig. 3 – Egg yolks are very rich in choline, an essential nutrient in the prevention and treatment of NAFLD.
Is there any medication for NAFLD?
Metformin and thiazolidinediones are pharmaceutical agents that promote insulin sensitivity in the body and have some utility in the treatment of NAFLD, particularly in diabetic patients.
Botanical agents such as berberine, milk thistle, and green tea extract have also been shown to be effective in clinical trials.
Several other substances, such as bile acid receptor agonists, are being actively researched for the treatment of NAFLD, but their clinical use is not recommended yet.
NAFLD is a condition that deserves the attention of all clinicians because of its growing prevalence and the severe consequences it can have, including the increased cardiovascular risk. Its silent character makes this condition especially dangerous, but it is entirely reversible, in its earliest stages, with a change in eating and lifestyle habits.
References:
Muhammad, A. Non-Alcoholic Fatty Liver Disease, an Overview. Integrative Medicine (Encinitas). 2019;18(2):42-49.
El-Agroudy NN, Kurzbach A, Rodionov RN, et al. Are Lifestyle Therapies Effective for NAFLD Treatment? Trends in Endocrinology and Metabolism, August 2019.
Akshintala D, Chugh R, Amer F, Cusi K. Nonalcoholic Fatty Liver Disease: The Overlooked Complication of Type 2 Diabetes. In: Feingold KR, Anawalt B, Boyce A, et al., eds. South Dartmouth (MA); 2000.
Masterjohn, C (2011). Non-Alcoholic Fatty Liver Disease. Retrieved from www.westonaprice.org/health-topics/nonalcoholic-fatty-liver-disease